27 yo CM, morbidly obese is seen for preoperative evaluation for Roux-en-Y gastric bypass surgery. He has suffered from obesity for many years and has tried numerous weight-reduction programs with no success. His current weight is 395 pounds, and his height is 5 feet, 11 inches. He denies any symptoms of chest pain, palpitations, heart murmurs or irregular pulse. No history of orthopnea. He has exertional dyspnea. No history of asthma, emphysema or chronic cough. No history of smoking.
PMH:
Obesity, OSA (a sleep study was ordered), DJD, psoriasis
SH:
Denies any history of alcohol, tobacco or illicit drugs.
FH:
Father has OSA.
Medications:
Motrin PRN, HCTZ
Physical examination:
VS 36.8-16-84-133/85
Morbidly obese, in NAD
The rest of the examination is unremarkable.
EKG: NSR, HR 79, left axis.
What happened?
He had a sleep study which conformed the clinical suspicion of OSA. The recommended setting was CPAP 10 cm H2O QHS. The first step in treating OSA is to find the right CPAP setting. The second is to find the device that fits the patient and is tolerated. Nasal trumpets are tolerated best but they cannot deliver pressure higher than 10 cm H2O. The full face mask is the most effective device, delivering pressure up to 20 cm H20, but many patients experience claustrophobia, find it very uncomfortable, and for these reasons, do not use it.
Sleep Study Report
Weight (lbs) = 406
Height = 70
Study type: SPLIT NIGHT PSG
Indications: Loud snoring, excessive daytime sleepiness.
ESS = 6
PMH: morbid obesity
Medications: Ambien given for the test
He is undergoing preop evaluation for bariatric surgery
PROCEDURE
An overnight/daytime full montage split night polysomnography was performed, recording EEG, EOG, chin and leg EMG, EKG airflow, thoracic and abdominal effort, snoring via a microphone, pulse oximetry, body positioning and CPAP pressure.
SLEEP ARCHITECTURE=
Total recording time=395
sleep efficiency was=increased
Sleep efficiency (normal about 85%)=96
Sleep latency was=reduced
Sleep Latency in minutes (normal 15-20 min)=3
Sleep architecture revealed=reduced amounts of REM sleep
REM % of TST (normal=20% of TST)=0.5
REM latency was=REM was absent
(Normal REM latency 70-120 min)=66
REM rebound was seen on CPAP
RESPIRATORY SUMMARY:
At (cmH20) =0
L/min O2 =0
Baseline SpO2 %=97
Min SpO2 %=87
NREM AHI=109
REM AHI=240
Overall RDI=112
Overall AHI=110
Respiratory Index=2
Obstructive apneas=38
Central Apneas=0
Hypopneas=158
Respiratory Effort Related Arousals (RERAS)=4
SNORING DATA:
Snoring without CPAP (% of sleep time)=49
Snoring was reported as=loud
CPAP ANALYSIS:
CPAP titration was started at=5
CPAP/BiPAP final pressure=13
In this study the most adequate pressure was=10
Higher pressures =no significant benefit
IMPRESSION:
Obstructive Sleep Apnea with hypersomnia
OSA=severe
RECOMMENDATIONS:
Avoid sedatives, hypnotics and narcotics=unless sleep apnea treated.
CPAP/BIPAP cm H20=10.
Do not operate heavy machinery or drive=unless OSA/other sleep disorder treated
Weight reduction=to IBW
Heated humidifier=with CPAP
What happened next?
He has been on CPAP for 2 weeks and today he had a Roux-en-Y gastric bypass surgery 2 hours ago.
He has been on CPAP for more than one week, VS are stable and he can be transferred to RMF.
What did we learn from this case?
The most important parameter for diagnosing OSA is AHI (Apnea-Hypopnea Index). In healthy people AHI is less than 10.
If you have to choose just one number to diagnose OSA, choose AHI. As a single measurement AHI is comparable to the importance of RSBI in weaning and extubation. RSBI of less than 100 predicts the successful extubation of a ventilated patient in 85 percent of the cases.
This is a simple bedside evaluation for OSA:
Physical exam - just check two things:
-Neck size
The risk size for OSA is 17' for men, and 16' for women
-Look inside the patient's mouth: "Open your mouth please" and check the the Mallampati Score (MS)
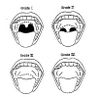
Mallampati Score (source: med.univ-rennes1.fr)
History:
-Epworth Sleepiness Scale (ESS), if more than 12, the patient is at high risk for OSA
References:
Obstructive Sleep Apnea-Hypopnea Syndrome - eMedicine
Snoring and Obstructive Sleep Apnea, Upper Airway Evaluation - eMedicine
Epworth Sleepiness Scale - University of Maryland, SMMC.com,
Treatment of Obstructive Sleep Apnea in Primary Care - AFP 02/04
Obstructive Sleep Apnea - AFP 11/99
Dr. Magboul Anesthesia page - MSN
Obstructive Sleep Apnea as a Risk Factor for Stroke and Death - NEJM 11/05
Continuous Positive Airway Pressure for Central Sleep Apnea and Heart Failure - NEJM 11/05
Sleep — A New Cardiovascular Frontier - NEJM Editorial 11/05
PMH:
Obesity, OSA (a sleep study was ordered), DJD, psoriasis
SH:
Denies any history of alcohol, tobacco or illicit drugs.
FH:
Father has OSA.
Medications:
Motrin PRN, HCTZ
Physical examination:
VS 36.8-16-84-133/85
Morbidly obese, in NAD
The rest of the examination is unremarkable.
EKG: NSR, HR 79, left axis.
What happened?
He had a sleep study which conformed the clinical suspicion of OSA. The recommended setting was CPAP 10 cm H2O QHS. The first step in treating OSA is to find the right CPAP setting. The second is to find the device that fits the patient and is tolerated. Nasal trumpets are tolerated best but they cannot deliver pressure higher than 10 cm H2O. The full face mask is the most effective device, delivering pressure up to 20 cm H20, but many patients experience claustrophobia, find it very uncomfortable, and for these reasons, do not use it.
Sleep Study Report
Weight (lbs) = 406
Height = 70
Study type: SPLIT NIGHT PSG
Indications: Loud snoring, excessive daytime sleepiness.
ESS = 6
PMH: morbid obesity
Medications: Ambien given for the test
He is undergoing preop evaluation for bariatric surgery
PROCEDURE
An overnight/daytime full montage split night polysomnography was performed, recording EEG, EOG, chin and leg EMG, EKG airflow, thoracic and abdominal effort, snoring via a microphone, pulse oximetry, body positioning and CPAP pressure.
SLEEP ARCHITECTURE=
Total recording time=395
sleep efficiency was=increased
Sleep efficiency (normal about 85%)=96
Sleep latency was=reduced
Sleep Latency in minutes (normal 15-20 min)=3
Sleep architecture revealed=reduced amounts of REM sleep
REM % of TST (normal=20% of TST)=0.5
REM latency was=REM was absent
(Normal REM latency 70-120 min)=66
REM rebound was seen on CPAP
RESPIRATORY SUMMARY:
At (cmH20) =0
L/min O2 =0
Baseline SpO2 %=97
Min SpO2 %=87
NREM AHI=109
REM AHI=240
Overall RDI=112
Overall AHI=110
Respiratory Index=2
Obstructive apneas=38
Central Apneas=0
Hypopneas=158
Respiratory Effort Related Arousals (RERAS)=4
SNORING DATA:
Snoring without CPAP (% of sleep time)=49
Snoring was reported as=loud
CPAP ANALYSIS:
CPAP titration was started at=5
CPAP/BiPAP final pressure=13
In this study the most adequate pressure was=10
Higher pressures =no significant benefit
IMPRESSION:
Obstructive Sleep Apnea with hypersomnia
OSA=severe
RECOMMENDATIONS:
Avoid sedatives, hypnotics and narcotics=unless sleep apnea treated.
CPAP/BIPAP cm H20=10.
Do not operate heavy machinery or drive=unless OSA/other sleep disorder treated
Weight reduction=to IBW
Heated humidifier=with CPAP
What happened next?
He has been on CPAP for 2 weeks and today he had a Roux-en-Y gastric bypass surgery 2 hours ago.
He has been on CPAP for more than one week, VS are stable and he can be transferred to RMF.
What did we learn from this case?
The most important parameter for diagnosing OSA is AHI (Apnea-Hypopnea Index). In healthy people AHI is less than 10.
If you have to choose just one number to diagnose OSA, choose AHI. As a single measurement AHI is comparable to the importance of RSBI in weaning and extubation. RSBI of less than 100 predicts the successful extubation of a ventilated patient in 85 percent of the cases.
This is a simple bedside evaluation for OSA:
Physical exam - just check two things:
-Neck size
The risk size for OSA is 17' for men, and 16' for women
-Look inside the patient's mouth: "Open your mouth please" and check the the Mallampati Score (MS)
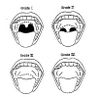
Mallampati Score (source: med.univ-rennes1.fr)
History:
-Epworth Sleepiness Scale (ESS), if more than 12, the patient is at high risk for OSA
References:
Obstructive Sleep Apnea-Hypopnea Syndrome - eMedicine
Snoring and Obstructive Sleep Apnea, Upper Airway Evaluation - eMedicine
Epworth Sleepiness Scale - University of Maryland, SMMC.com,
Treatment of Obstructive Sleep Apnea in Primary Care - AFP 02/04
Obstructive Sleep Apnea - AFP 11/99
Dr. Magboul Anesthesia page - MSN
Obstructive Sleep Apnea as a Risk Factor for Stroke and Death - NEJM 11/05
Continuous Positive Airway Pressure for Central Sleep Apnea and Heart Failure - NEJM 11/05
Sleep — A New Cardiovascular Frontier - NEJM Editorial 11/05