Author: V. Dimov, M.D.
Reviewer: S. Randhawa, M.D.
An 82-year-old AAM came to the hospital with CC: severe back pain for one week. He has prostate cancer diagnosed five years ago.
PMH
DM2, PUD S/P remote surgery, HTN, prostate cancer with bone mets, (B) orchiectomy.
Medications
Insulin, Bisacodyl, Senokot, Risperdal, Sertraline, metoclopramide, Benadryl, Docusate, Glipizide.
Physical exam
VS 37.3-108-16-125/80.
CVS: Clear S1S2.
Chest: CTA (B).
Abd: Soft, NT, ND, +BS.
Back: Limited ROM, no local tenderness.
Rectal exam: decreased sphincter tone, no blood. The prostate is big and hard.
Neuro: nonfocal.
What do you think is going on?
Progression of bone mets.
What tests would you order?
CBCD, CMP
MRI of the back

CMP shows elevated AP and PSA greater than 900 ng/mL, his DM is uncontrolled (HA1c 17) (click to enlarge the image).

Alkaline phosphatase levels over the last two years (click to enlarge the image).

PSA levels over the last two years (click to enlarge the image).


Bone scan from one year ago (click to enlarge the images).


CXR; Surgical scars from previous PUD surgery (click to enlarge the images).





Thoracic vertebra with osteoblastic mets; Close-up; MRI of the thoracic spine (click to enlarge the images).
MRI showed extensive bony metastatic disease in the lumbar spine as well as varying degrees of canal stenosis, most severe at level L3-L4 and foraminal stenosis was also noted at multiple levels.
MRI of thoracic spine with and w/o contrast
Findings: Comparison is made with the previous exam from one year ago. Sagital images demonstrate extensive heterogeneity of marrow signal throughout the thoracic spine, which would be consistent with multiple bony metastases. There is extensive abnormality of marrow signal involving the T10 vertebral body. There are less extensive lesions involving T9 and T11, also noted on the previous exam. Further lesions are noted more superiorly in the thoracic spine at this time, being most pronounced at the T2 and T4 levels, but also seen at several additional levels. No gross thoracic compression fracture is identified. The spinal cord does not appear abnormally widened. No cord compression is seen. No focal cord enhancement is identified. There are multiple enhancing vertebral lesions. If clinically indicated, post myelographic CT might permit better definition of the thoracic cord and spinal canal.
Impression:
1. Extensive bony metastatic disease throughout the thoracic spine, appearing more widespread than on the previous study; similar appearance noted that T9, T10 and T11 levels.
2. No abnormal widening of the thoracic cord and no focal cord enhancement identified.
4. Bony canal stenosis suspected at the T10 level, relating to posterior element disease; no cord compression identified

MRI of the lumbar spine shows extensive metastatic disease (click to enlarge the images).

MRI of the lumbar with bone mets (click to enlarge the image).
MRI of lumbar spine with and w/o contrast
Findings: There is severe degenerative narrowing of the L5-S1 disc interspace, with associated degenerative endplate changes, particularly involving L5. There is diffusely diminished signal with some heterogeneity involving the L4 vertebral body, suggesting diffuse marrow infiltrating pathology. More focal lesions are noted in the remaining vertebral bodies, with a focal rounded lesion overlying the superior L2 vertebral body, of diminished T1 and increased T2 signal, where enhancement is also noted. These findings suggest diffuse bony metastatic disease in the lumbar spine. Further focal lesions overlying the visualized sacrum bilaterally, with further involvement of the iliac bones suspected posterior medially, again suggesting the bony metastatic disease. No compression of the conus is seen.
At L3-4 there is severe canal stenosis, in association with posterior element hypertrophy and relatively short pedicles.
Impression:
1. Extensive bony metastatic disease in the lumbar spine, as described above; concern for mild increase in AP diameter of the L4 vertebral body.
2. Varying degrees of canal stenosis, as described above, being most severe at the L3-4 disc level.
3. Foraminal stenosis also noted at multiple levels, most severe at the lower three lumbar disc levels.
4. Further metastatic lesions in the visualized sacrum and iliac bones. These findings might be better evaluated globally by bone scan.
What happened?
A Fentanyl patch was started and the pain decreased to 1/10. Patient felt much better, oncology consult was called and he was discharged to a transitional care unit. He refused treatment for his prostate cancer.
Final diagnosis
Prostate cancer with extensive bony metastases to the thoracic and lumbar spine.
Published: 03/09/2004
Updated: 08/12/2005
Reviewer: S. Randhawa, M.D.
An 82-year-old AAM came to the hospital with CC: severe back pain for one week. He has prostate cancer diagnosed five years ago.
PMH
DM2, PUD S/P remote surgery, HTN, prostate cancer with bone mets, (B) orchiectomy.
Medications
Insulin, Bisacodyl, Senokot, Risperdal, Sertraline, metoclopramide, Benadryl, Docusate, Glipizide.
Physical exam
VS 37.3-108-16-125/80.
CVS: Clear S1S2.
Chest: CTA (B).
Abd: Soft, NT, ND, +BS.
Back: Limited ROM, no local tenderness.
Rectal exam: decreased sphincter tone, no blood. The prostate is big and hard.
Neuro: nonfocal.
What do you think is going on?
Progression of bone mets.
What tests would you order?
CBCD, CMP
MRI of the back

CMP shows elevated AP and PSA greater than 900 ng/mL, his DM is uncontrolled (HA1c 17) (click to enlarge the image).

Alkaline phosphatase levels over the last two years (click to enlarge the image).

PSA levels over the last two years (click to enlarge the image).


Bone scan from one year ago (click to enlarge the images).


CXR; Surgical scars from previous PUD surgery (click to enlarge the images).





Thoracic vertebra with osteoblastic mets; Close-up; MRI of the thoracic spine (click to enlarge the images).
MRI showed extensive bony metastatic disease in the lumbar spine as well as varying degrees of canal stenosis, most severe at level L3-L4 and foraminal stenosis was also noted at multiple levels.
MRI of thoracic spine with and w/o contrast
Findings: Comparison is made with the previous exam from one year ago. Sagital images demonstrate extensive heterogeneity of marrow signal throughout the thoracic spine, which would be consistent with multiple bony metastases. There is extensive abnormality of marrow signal involving the T10 vertebral body. There are less extensive lesions involving T9 and T11, also noted on the previous exam. Further lesions are noted more superiorly in the thoracic spine at this time, being most pronounced at the T2 and T4 levels, but also seen at several additional levels. No gross thoracic compression fracture is identified. The spinal cord does not appear abnormally widened. No cord compression is seen. No focal cord enhancement is identified. There are multiple enhancing vertebral lesions. If clinically indicated, post myelographic CT might permit better definition of the thoracic cord and spinal canal.
Impression:
1. Extensive bony metastatic disease throughout the thoracic spine, appearing more widespread than on the previous study; similar appearance noted that T9, T10 and T11 levels.
2. No abnormal widening of the thoracic cord and no focal cord enhancement identified.
4. Bony canal stenosis suspected at the T10 level, relating to posterior element disease; no cord compression identified
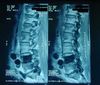
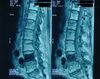

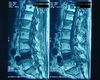
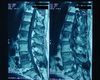
MRI of the lumbar spine shows extensive metastatic disease (click to enlarge the images).

MRI of the lumbar with bone mets (click to enlarge the image).
MRI of lumbar spine with and w/o contrast
Findings: There is severe degenerative narrowing of the L5-S1 disc interspace, with associated degenerative endplate changes, particularly involving L5. There is diffusely diminished signal with some heterogeneity involving the L4 vertebral body, suggesting diffuse marrow infiltrating pathology. More focal lesions are noted in the remaining vertebral bodies, with a focal rounded lesion overlying the superior L2 vertebral body, of diminished T1 and increased T2 signal, where enhancement is also noted. These findings suggest diffuse bony metastatic disease in the lumbar spine. Further focal lesions overlying the visualized sacrum bilaterally, with further involvement of the iliac bones suspected posterior medially, again suggesting the bony metastatic disease. No compression of the conus is seen.
At L3-4 there is severe canal stenosis, in association with posterior element hypertrophy and relatively short pedicles.
Impression:
1. Extensive bony metastatic disease in the lumbar spine, as described above; concern for mild increase in AP diameter of the L4 vertebral body.
2. Varying degrees of canal stenosis, as described above, being most severe at the L3-4 disc level.
3. Foraminal stenosis also noted at multiple levels, most severe at the lower three lumbar disc levels.
4. Further metastatic lesions in the visualized sacrum and iliac bones. These findings might be better evaluated globally by bone scan.
What happened?
A Fentanyl patch was started and the pain decreased to 1/10. Patient felt much better, oncology consult was called and he was discharged to a transitional care unit. He refused treatment for his prostate cancer.
Final diagnosis
Prostate cancer with extensive bony metastases to the thoracic and lumbar spine.
Published: 03/09/2004
Updated: 08/12/2005